Healthcare companies are facing increasing levels of scrutiny over the last few years. Compliance for healthcare companies now covers a wider scope of aspects—bringing in healthcare providers, third, and fourth-party vendors that work with health care providers under its purview.
According to research by the Ponemon Institute published by IBM, the average cost of healthcare data breaches has seen a 53% jump since 2020 making it the most expensive industry for data breaches, 13th year in a row!
A number of new progressive disruptions, such as the rapid adoption of online consultations and telehealth services, have brought along new privacy and security challenges. Malicious actors are now looking to exploit patient information that is available online. This is one of many new instances that compliance aims to fix in the realm of healthcare.
This blog lists the steps to get you started on healthcare compliance laws and lays down a few healthcare compliance examples you need to follow.
TL;DR:
| Compliance in healthcare ensures adherence to regulatory and ethical standards that protect sensitive information and eliminate instances of fraud and security events. |
| To get compliant in healthcare, your organization must formulate a compliance program, outline policies, conduct workforce training, create communication channels, and enable continuous compliance |
| Some healthcare compliance laws include HIPAA, HITECH, Stark law, False Claims Act, EMTALA, and ACA. |
What is Healthcare Compliance?
Healthcare compliance refers to a set of processes that ensure organizations adhere to legal, professional, and regulatory standards aimed at minimizing fraud, waste, and abuse in the healthcare industry, as well as protecting sensitive medical information.
It is regulated by authorities and organizations at different levels like federal, state, local entities, industry-specific organizations, and accreditation bodies to ensure safe and ethical practices in healthcare.
Why is compliance important in healthcare?
Compliance is important in healthcare to avoid substandard service delivery, unintentional or intentional deception, negligence in patient care, compromise of patient data privacy, and unethical practices.
Globally, there are multiple compliance regulations and laws that aim to protect the integrity of patient data. Becoming compliant with these regulatory laws is the first major check item for any organization that is a healthcare organization or is working with one.
Healthcare compliance is critical in safeguarding federal, state, and commercial insurance funds from misuse. Its primary purpose is to prevent the submission of erroneous claims to healthcare insurance carriers across all sectors. It aims to mitigate risks associated with fraud, waste, and abuse.
Here’s why compliance for healthcare matters:

- The enormous size of the healthcare industry and the sensitivity of services provided expose it to substantial risks. This is due to data passing through various hands, making compliance a crucial concern.
- Healthcare services directly affect human lives, making it important to uphold standards of integrity for patients to be safe.
- Maintaining the confidentiality, integrity and availability of PHI (protected health information) is important for protecting patient rights, privacy and trust.
- Compliance ensures the minimization of fraud and ensures proper utilization of funds.
- Data breaches can cost organizations money, disrupt business continuity, tarnish brand image, and strain customer relationships
- Compliance programs help proactively identify vulnerabilities and helps prevent or reduce the impact of incidents
- Compliance fosters an environment of trust amongst stakeholders and clients and brings better business opportunities.
Check out: Complete Guide to HIPAA compliance
What is the scope of healthcare compliance?
The scope of compliance for healthcare is vast and can vary based on factors like geographical location, type of healthcare organization, and service provided. While it includes regulatory compliance, billing and coding practices, ethical research, and patient care, it is also constantly shaped by the evolving nature of risk, and changes in laws and standards.
Key Elements of Healthcare Compliance
A successful healthcare compliance program hinges on five key elements that integrate processes to create a culture of compliance within the organization. These elements provide the foundation for ensuring regulatory adherence and risk mitigation.
Let’s delve into how these elements function and their role in enhancing your compliance according to the inputs from our compliance experts.
1. Risk Assessments
Healthcare risk assessment is not simply a compliance exercise where one identifies risks and corrects them. It spots potential problems that could disrupt patient care, safety, or daily operations. The goal is simple—to figure out what could go wrong, assess how likely and serious those risks are, and take steps to prevent or minimize them.
But are we peering down far enough? Risk assessments push organizations to ask hard questions:
- What is the adequacy of existing measures?
- What annexations might still be possible?
- All operational processes, from process flows to third-party vendors, are analyzed to prevent risk before it becomes an issue.
For instance, it becomes challenging when there are new layers, such as managing cloud-based software and interacting with contractors. Ad hoc risk assessment practices lead to vulnerabilities, which often make the organization blind to actual risks.
Thus, tools like Sprinto combine all these risks into one window with data that can be easily leveraged by teams to safeguard operations and patients.
2. Employee training
This healthcare training develops competent, confident human resource personnel who are thus prepared to respond to any situation.
Are your employees ready to confront the challenges of patient care, infection control, or compliance audits?
A great training program includes:
- When the employees are aware of the recommendations, the patient receives standard care from the health facility.
- Correct training has a way of discharging your organization’s liability limit and steering clear of legal troubles.
- When learning is standardized, it implies fewer errors, less repetition, and more efficient workers in the organization.
- It is not mysterious to anyone and everyone knows what he or she is supposed to do in a given task.
- That’s why when employees are informed, they are assured and able to deliver.
Sprinto Advantage
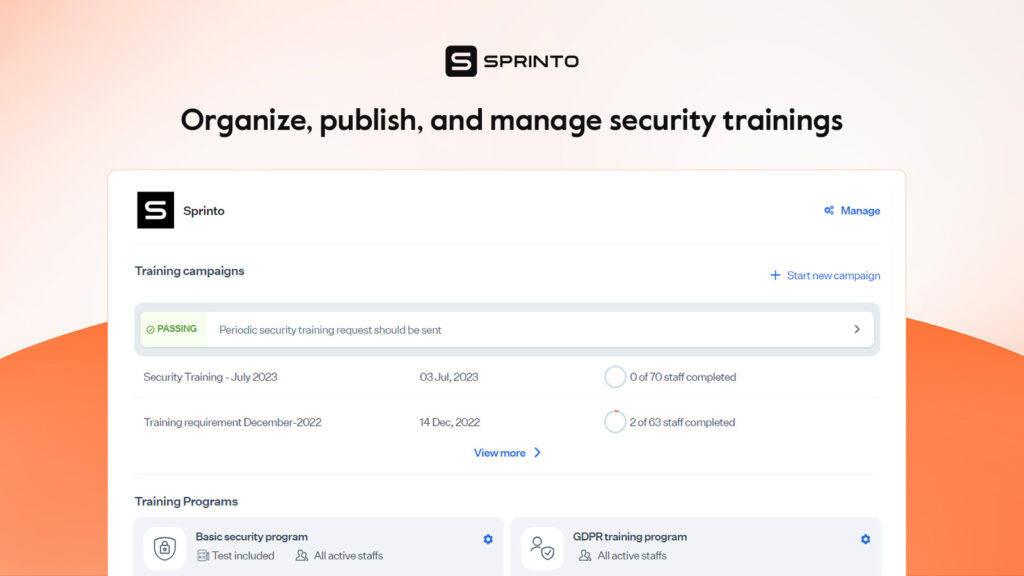
Sprinto makes cybersecurity training easy. With built-in, compliance-aligned courses, you can launch engaging training programs that quickly and effortlessly get your team on the same page.
Already have a training program in place? No problem!
Sprinto integrates with top training providers, making managing and boosting participation easier. It all remains steady and centralized so you can literally monitor training progress in real time, check up on control checks with handy alerts and even collate compliance evidence without exerting yourself.
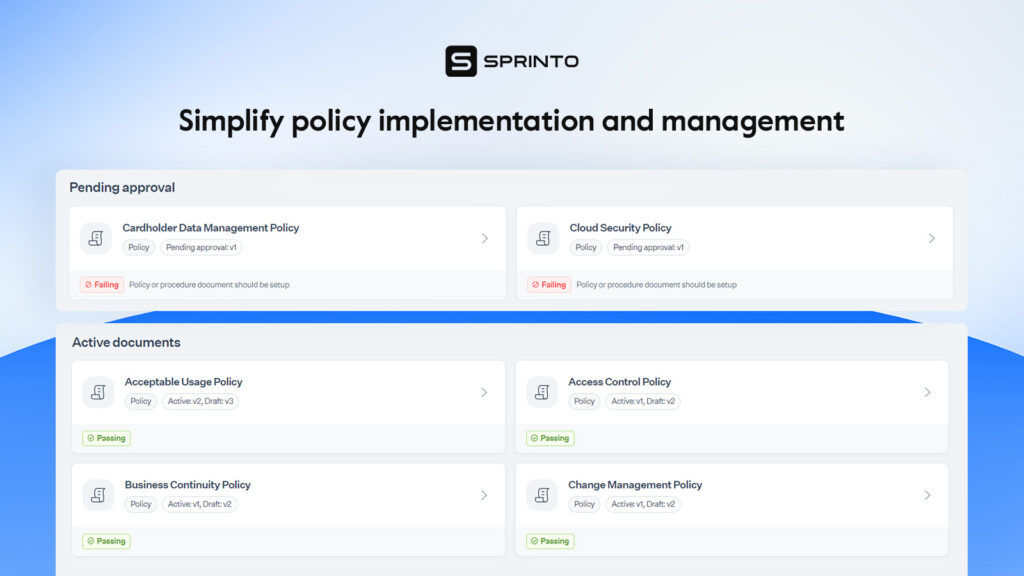
3. Policies
Research shows that many organizations (69%) rely on multiple tools to manage this complex process. Alarmingly, 43% of organizations still use paper signatures, which raises questions about the efficiency and security of their policy management.
In the context of healthcare cybersecurity, a policy can be defined as written protocols that include a clear course of action regarding the management of and protection of information.
Developing such policies and ensuring they remain current with current practices can be challenging. Healthcare organizations must ensure their policies are active, relevant, and compliant, requiring constant vigilance.
So, what policies should be at the forefront of any healthcare cybersecurity plan? Here are some crucial ones:
- Access Control Policy
- Data Encryption Policy
- Incident Response Policy
- Password Management Policy
- Employee Training and Awareness Policy
- Remote Access Policy
- Data Backup and Recovery Policy
- Third-Party Vendor Management Policy
- Privacy and Confidentiality Policy
- Audit and Monitoring Policy
4. Internal Audits
Internal audits are essential when it comes to compliance issues in healthcare facilities. The main purpose of these audits is to determine whether healthcare providers are following legal requirements and/or regulations. It is, therefore, important to note that while regulatory audits may descend on the company unannounced, internal ones do not afford the same luxury.
Notably, some regulatory bodies provide 7 to 60 days of notice; meanwhile, internal audits guarantee better risk management and problem-solving.
Remember, documentation is crucial; if it’s not in writing, it’s as if it never happened.
A platform like Sprinto can significantly ease the internal audit process. With features like automated reporting, centralized document management, and compliance tracking, Sprinto streamlines the monitoring of policies and procedures.
5. Incident management
Incident management refers to the structured processes and procedures employed to identify, assess, and mitigate organizational hazards. It’s basically designed to address current incidents and prevent recurrence through thorough analysis and corrective action.
Key threats that must be identified and managed include:
- HIPAA Violations: Situations involving violation of patient’s privacy rights or health information security.
- Cybersecurity Attacks: Cyber attacks, threats, and even malware that violates data or information technology assets.
- Physical Hazards: These may cause slips, trips, and falls that could lead to injuries.
- Accidental Needlesticks: Hazard caused by improper use of sharps.
- Chemical Exposures: In contact with endangering influences, hazardous material is acquired.
- Theft, Vandalism, or Loss: Trespass, loss, or damage to or destruction of physical or data assets.
- Workplace Violence: Violence is perpetrated within healthcare facilities regardless of the inviolable nature of the place.
- Natural Disasters: Situations in which ongoing business activities are disrupted by events like earthquakes, floods, or fires.
- Human Error: Measures that personnel can take and produce unfavorable conditions or consequences to the organization.
- Network or Technological Failures: Disruptions of the normal operational process, information access, or communication ability.
You can access our Incident Management Policy Template below.
Download Your Incident Management Policy Template
Who regulates healthcare compliance?
Healthcare compliance is regulated by agencies at the federal level and state level. Some of these key regulators include:
- Department of Health and Human Services (HHS): Oversees healthcare programs and regulations such as HIPAA
- Office for Civil Rights (OCR): Ensures HIPAA enforcement to maintain patient data privacy and security
- Office of Inspector General (OIG): Monitors any fraud, abuse and misuse in healthcare programs with HHS
- The Joint Commission (TJC): Accredits and certifies healthcare organizations in the U.S.
- Center for Medicare and Medicaid Services (CMS): Works in quality initiatives through Medicare and Medicaid programs
- Drug Enforcement Administration (DEA): Enforces controlled substances regulations
- Food and Drug Administration (FDA): Ensures the safety and security of drugs, medical devices, and food supply
How to get started with compliance for healthcare?
At the outset, healthcare compliance can pose practical challenges. It requires an understanding of the persistent risks, selecting a framework, training the workforce, establishing communication channels, and tracking progress. However, when done right, it can save the organization from various non-compliance repercussions.
Here’s how organizations can get compliant in healthcare:

Prepare for the program
The preliminary work when initiating compliance for healthcare involves conducting a risk assessment to understand risk profile. Thereafter, a healthcare compliance program must be designed with the right protocols, implementation, communication channels and perpetual improvements.
Outline policies and procedures
Once the organization understands its current state and areas that need to be addressed, it must pick a framework. A hospital, for example, will begin by implementing HIPAA standards.
Next, the chosen framework must be mapped to policies, processes and people. This will bring clarity regarding the creation, revision, alteration or reinstatement of policies.
The policies must be regularly reviewed and updated to reflect changes in regulations, advancements or organizational requirements and they must be acknowledged by employees.
You don’t have to create these policies from scratch. Instead, leverage Sprinto’s HIPAA-aligned policy templates to fast-track the process.
Set up program administration
The next step is to designate a compliance officer for program oversight, implementation and point of contact. This includes monitoring regular activities, assessing program effectiveness, tracking regulatory changes, reviewing reports, arranging employee training, and ensuring smooth audits.
On the external front, the compliance officer is required to have communication with vendors to periodically run third-party compliance checks, seek legal counsel, and liaise with auditors and regulatory bodies.
Arrange for workforce training
Workforce training is an essential aspect of healthcare compliance. Employees should be aware of best practices while handling sensitive PHI such as patient access, and breach notification. They must know how to identify and communicate non-compliance and put containment actions in place.
Training programs must be designed by designation. This ensures each person understands their role within the function. Examples of such training modules include compliance training, fraud prevention, and incident management.
While these training programs can cost you $1-$2 per employee if you get them outsourced from a company, Sprinto offers in-built HIPAA training modules for free. The platform also lets you track completion rates and nudge employees to complete training modules.
Set up communication channels
For this step, two communication pathways need to be set up: internal and external. The internal channels should facilitate escalation of any compliance compromises across departments. The aim of an internal channel is to ensure quick containment, seamless coordination, and quick resolution.
Next, a system should be established for receiving and responding to customer complaints through various channels like emails and online portals. The idea is to proactively communicate with customers whenever needed.
Conduct regular reviews and audits
More often than not, opting for a third-party audit without having internal audits and assessments does not work out in the organization’s favor. Regular reviews and internal audits must be a regular practice for progress visibility and process improvement. It serves as a litmus test of the strength of controls put in place.
You can create an internal audit window on the independent audit dashboard with Sprinto and verify evidence against controls. Once assured of crossing the >90% mark, apply for a certification.
Work on sustained progress
In order to maintain the highest standards of adherence, the compliance officer must demonstrate strong leadership and governance. Regular risk assessments, continuous compliance tracking, solid documentation, and a robust response mechanism are the pillars of sustained progress.
You can make use of an automation software like Sprinto for tracking compliance status, gaps and progress. The health dashboard will give you a quick snapshot of passing, failing, critical and due checks to ensure quick responses and no compliance drift.
Also, before you begin setting up a compliance program, it is important you grasp certain healthcare compliance laws to select the right one. Let’s discuss them in the next section.
Check out: HIPAA compliance checklist
Healthcare compliance laws
The health industry is governed by several laws and regulations with the overarching objectives of providing quality healthcare services and ensuring the safety of patient data. Each of these laws has its own set of requirements and ensure compliance across different concerning areas.
Some key healthcare compliance laws include:

1. Health Insurance Portability and Accountability Act (HIPAA)
HIPAA is a federal law enacted in 1996 that requires organizations working directly or indirectly in a healthcare capacity to maintain the confidentiality, integrity, and availability of PHI (Patient health information). The law grants certain rights to patients to ensure that any sensitive information is not accessed or disclosed by unauthorized users.
2. Health Information Technology for Economic and Clinical Health (HITECH) Act
The HITECT Act of 2009 aims to increase the adoption of electronic health records (EHR) and the effective utilization of health information technology (HIT) within the US healthcare system. It is a part of the American Recovery and Reinvestment Act (2009) and promotes healthcare efficiency and patient safety.
3. Emergency Medical Treatment and Labour Act (EMTALA)
Enacted in 1986, EMTALA act requires hospitals to provide the necessary treatment to a patient who arrives at the emergency department or arrange for an appropriate transfer for stabilization. The screening and stabilization can’t be refused for any discriminatory reason like an inability to pay. The act safeguards patient rights and ensures equitable access to emergency services.
4. Patient Protection and Affordable Care Act (ACA)
The Patient Protection and Affordable Care Act known as ACA or Obamacare aims to improve access to quality healthcare by making it affordable for low-income groups. It ensures subsidies, access to affordable health insurance, and medical aid to households living below the federal poverty line.
5. Anti-Kickback Statute (AKS)
The Anti-Kickback Statute is a federal law that prohibits the offer/payment/receipt of any kind of remuneration in exchange for referrals or business generation including services reimbursed by Federal health care programs. It aims to combat healthcare fraud and abuse and can lead to civil and criminal penalties.
6. Stark law
Also known as the Physician Self-referral law, the Stark law prohibits physicians from referring patients to receive designated health services (DHS) reimbursed by Medicare or Medicaid to entities with whom they or their immediate family members have financial relationship. Examples of designated health services include clinical laboratory services, home health services, etc.
7. False Claims Act
The False Claims Act in the United States imposes a liability of three times the government damages and other penalties linked to inflation on individuals submitting or causing to submit false claims to the federal government.
On the other hand, it also provides a percentage of monetary recovery to individuals filing successful lawsuits on behalf of the government for such false claims, under its qui tam provisions.
8. GDPR
The General Data Protection Regulation (GDPR) is a data protection law that is also relevant to the healthcare industry. The law protects personal data of EU citizens including sensitive health information which is a category under the law.
US healthcare entities handling Personal Health Information of EU patients must strictly comply with GDPR regulations and protect patient rights.
8. CCPA
The California Consumer Privacy Act (CCPA), similar to the GDPR, is a privacy law that protects the rights of California residents over their personal information. Healthcare entities dealing with sensitive patient data for California residents must adhere to the CCPA and disclose their data practices when required.
Additionally, for companies outside the scope of HIPAA—such as a fitness app—the CCPA grants California residents the right to request the deletion of their data or to opt out of targeted marketing campaigns.
Coming up next is how these laws are put into practice at healthcare organizations. Check out healthcare compliance examples below.
Healthcare compliance examples
Any task or activity executed in good faith ensuring the adherence to legal, ethical, and professional standards in the healthcare industry is compliance for healthcare. This includes following regulations, ensuring patient safety and privacy, maintaining quality services, and abiding by medical ethics.
Some examples of healthcare compliance include:
- Hospitals implementing a security policy that defines restrictions on access to PHI and unauthorized disclosure
- Clinical laboratories maintaining quality standards for reliable testing
- Healthcare entities adhering to billing and coding practices to prevent fraudulent activities
- Healthcare organizations ensuring safety and well-being of employees and patients
- Pharmacies signing Business Associate Agreement with third-parties
- Healthcare providers implementing physical, technical and administrative safeguards to secure e-PHI.
- Physicians not indulging in any unethical referral or business generation activity in which they have financial interest.
The consequences of non-compliance
Non-compliance in healthcare can lead to severe financial and legal consequences, significantly impacting an organization’s stability and reputation. Here’s a summary of the key consequences:
- Fines: Regulatory bodies, like OCR, can impose fines ranging from thousands to millions of dollars.
- Settlement Costs: Lawsuits related to non-compliance can drain resources and divert funds.
- Revocation of Funding: Losing federal funding can lead to service cuts, layoffs, and even closure.
- Legal Consequences: Criminal charges, civil lawsuits, and license revocation can result in long-term financial and reputational damage.
Estimated Costs
| Category | Estimated Costs |
| Fines | $10,000 to $50 million+ |
| Settlement Costs | Varies: typically $100,000 to millions |
| Revocation of Funding | Loss of millions in federal/state support |
| Criminal Charges | Imprisonment for individuals; fines up to $500,000 |
| Civil Lawsuits | Legal costs: $50,000 to several million |
| Loss of Licenses | Loss of revenue, permanent shutdown risks |
Automate healthcare audit end-to-end
Ace healthcare compliance with Sprinto
Compliance for healthcare is multi-faceted and challenging. It requires the most stringent adherence to several constantly evolving regulations while keeping pace with technological advancements. It also demands a very high level of collaboration to manage investigations, conduct audits, coordinate with third-party vendors, etc.
A comprehensive healthcare compliance tool like Sprinto helps you every step of the way. With our powerful platform, you can align your organizations with the requirements of various frameworks, establish best practices, leverage pre-built policy templates, automate evidence collection and more.
Looking for expert advice? We have you covered. Speak to our healthcare compliance experts today.
FAQs
What are the three main areas of healthcare compliance?
The three main areas of healthcare compliance are patient safety, patient privacy and data security and billing and coding compliance.
What is an example of patient compliance?
Patient compliance or patient adherence is the degree to which a patient follows the prescribed medical treatment by the healthcare provider. An example is if the patient is prescribed a medicine for a chronic disease twice a day along with regular exercise and he follows the guidelines as instructed, the patient is compliant.
What is the Patient Safety and Quality Improvement Act (PSQIA)?
The Patient Safety and Quality Improvement Act (PSQIA) is a federal law enacted in 2005 that establishes a framework for Patient Safety Organizations (PSOs) when collecting patient safety data from healthcare providers. It ensures that the data reported to PSO by healthcare organizations is not used in lawsuits or legal proceedings and encourages a culture of transparency.
What are the reporting requirements for data breach under HIPAA?
In the case of a data breach under HIPAA, covered entities must notify the affected individuals, the Department of Health and Human Services (HHS), and, in some cases, the media. If the breach affects 500 or more individuals, the notification must be provided without unreasonable delay and no later than 60 days after the breach’s discovery.
What are some sources for healthcare compliance training?
Some popular sources for healthcare compliance training include Accountable HQ, Biologix solutions, Coursera and ProTrainings. You can also leverage in-built HIPAA training modules from GRC tools like Sprinto.
Payal Wadhwa
Payal is your friendly neighborhood compliance whiz who is also ISC2 certified! She turns perplexing compliance lingo into actionable advice about keeping your digital business safe and savvy. When she isn’t saving virtual worlds, she’s penning down poetic musings or lighting up local open mics. Cyber savvy by day, poet by night!
Explore more
research & insights curated to help you earn a seat at the table.