Risk Management in Healthcare: Strategies for a Safer Future

The healthcare sector has seen immense efficiency gains from technology—improved patient outcomes, centralized services through third-party vendors, better data management, and a constant drive for innovation. However, beneath the benefits lie a complex web of interconnected challenges—regulatory laws, clinical issues, patient data concerns, and an under-preparedness for cyber attacks. It’s no wonder that year after year, healthcare is flagged as one of the riskiest industries. The need for effective risk management in this field couldn’t be more apparent.
In this blog, we discuss the pressing risks that the healthcare industry faces and the steps to create a future-proof risk management plan.
TL;DR
| Risk management in healthcare is crucial to optimize patient care, ensure compliance, maintain a positive public perception, and embrace innovation. |
| The risk domains to focus on for the healthcare industry include operational, clinical, strategic, technological, financial, workplace safety, legal, cybersecurity, environmental, and third-party risks. |
| To create a risk management plan, organizations must identify potential risks, prioritize the ones that matter, develop mitigation plans, implement measures, train the workforce, document, monitor, and improve. |
What is risk management in healthcare?
Risk management in healthcare is the identification, assessment, and mitigation of risks that could compromise patient safety, hinder compliance, and impact the financial or operational stability of healthcare facilities. It helps minimize harm, capitalize on the right opportunities, and enhance trust in care delivery.
The value and purpose of risk management in healthcare
There are two sides to the healthcare industry story. On one side, the sector has already begun visualizing ‘smart healthcare’ as its future with AI technologies, personalized assistance, and enhanced infrastructure. Contrary to this, we have stats that tell us that 1 in 10 patients are harmed due to unsafe care, and 92% of healthcare organizations face a cyberattack. The contrasting realities underscore the need for robust risk management in healthcare, especially as the industry plans to embrace innovation.
Here’s why you need healthcare risk management:
Prioritizing patient care
Prioritizing patient safety is an ethical responsibility and a patient’s right. As an integrated process, risk management helps identify risks to patient safety, such as medical errors, equipment failures, and other adverse events. This enables healthcare organizations to proactively address issues and create a safer environment while delivering high-quality care.
Maintaining compliance
It’s safe to say that risk management forms the basis of adherence to compliance standards, including healthcare compliance. Risk assessments help identify threats to patient privacy (HIPAA, HITECH, etc.), billing records (False Claims Act), and the safety and efficacy of medical devices (FDA). Mitigation plans address these gaps and enable the organization to stay on track with applicable regulations while protecting it from fines and penalties.
Protecting financial health
Medical errors, unoptimized processes, or lawsuits due to non-compliance can impact an organization’s financial health. Foreseeing and addressing the risks in advance is the only way to protect against revenue loss. Here’s a simple example: Healthcare providers are reimbursed accurately when they adhere to billing standards set forth by the Center for Medicare and Medicaid Services (CMS). So, to avoid billing errors, the organization must implement risk management measures such as staff training and regular internal audits.
Optimizing operations
Risk management in healthcare helps reveal and address gaps in operational workflows, minimizing bottlenecks and redundant processes. It also enables better resource prioritization and well-informed decisions to improve overall performance. In the long term, though, you see ripple effects—smoother operations, cost efficiencies, and enhanced patient care.
Preserving reputation
When an organization’s key processes are on track, it upholds high standards of care delivery, allowing confidence to naturally grow and enabling stakeholder relationships. Overall, public perception improves as the organization is recognized for its strong commitment to security, compliance, and accountability.
Create and monitor a healthcare compliance program
Risk domains to focus for healthcare organisation
Healthcare risks are broad and understanding the risk domains makes it easier to implement targeted strategies and prioritize them better. Here’s a list of risk domains to focus on for any healthcare organization:

Operational
Operational risks are threats and vulnerabilities arising from mismanagement of day-to-day operations, systems, and resources, such as patient admission delays or record errors. These can also arise from clinical processes that directly impact patient safety or the quality of medical services such as a delay in treatment or an incorrect dosage.
Strategic
Strategic risks are linked to decisions made by executive management, any external forces or an unanticipated shift in the industry. They impact the organization’s ability to achieve long-term goals or maintain it’s market position. For example, loss of patient base due to competitors adopting AI-driven diagnostics.
Technological
Technological risks occur due to failures in technological systems that can impact operations, finances or the organization’s reputation. For example, lost data due to system failure.
Financial
Financial risks are uncertainties caused by an organization’s unstable financial health. These may be due to ineffective cost management or revenue shortfalls. Examples include reduced profit margins due to increased medical supplies costs or fines and penalties due to non-compliance with regulations.
Workplace safety
Workplace safety risks are potential hazards caused by faulty equipment, processes, or other inefficiencies in the work environment that can cause injury, illness, or health risks for staff, visitors, and even patients. For example, respiratory issues due to improper handling of hazardous chemicals.
Human capital
Human capital risks are challenges that arise due to talent shortages, retention and turnover, inadequate training, staff burnout and resistance to change. For example, workers lacking training in newly implemented diagnostic tools impacting patient care.
Legal and regulatory
Legal and regulatory risks arise due to non-compliance with healthcare laws, regulations, and industry standards, leading to lawsuits, penalties, and operational disruptions. For example, fines and penalties under HIPAA due to improper handling of patient data.
Third-party risks
Third-party risks in healthcare are due to reliance on vendors, partners or service contractors that can impact security, operations and compliance. For example, improper data protection measures by third-parties leading to HIPAA violations.
Cybersecurity risks
Cybersecurity risks are threats and vulnerabilities that impact the confidentiality, integrity, and availability of systems or data. They arise due to cyber attacks, breaches, human errors, and negligence and can significantly impact the organization. Examples include the use of weak passwords that lead to unauthorized access and the use of deceptive emails by cybercriminals for phishing attacks.
Manage risks unique to your business with precision
Steps to create a healthcare risk management plan
A healthcare risk management plan is a documented procedure for risk managers and relevant stakeholders. It helps the organization understand how to carry out risk identification, mitigation, and ongoing risk management.
Here’s a list of steps to create a healthcare risk management plan:

Identify potential risks
Start by establishing a business context by reviewing your current clinical practices, administrative operations, financial processes, and technological environment. To identify the potential risks, you can:
- Interview stakeholders from various departments such as IT, clinical, finance, etc.
- Conduct vulnerability scans and penetration tests
- Use risk management frameworks and tools used in the healthcare industry, such as Failure Mode and Effects Analysis (FMEA), Root Cause Analysis (RCA), risk registers etc.
Failure Mode and Effects Analysis (FMEA) involves identifying failures in clinical or healthcare processes before they occur and reducing the likelihood of adverse events. It determines various failure modes and helps pinpoint the underlying cause of each mode.
Root Cause Analysis (RCA) helps identify underlying causes for incidents or near misses that have previously occurred to develop solutions accordingly.
Risk registers track the different types of risks applicable to the organization and categorize them with unique IDs, descriptions, scores, impacts, etc.
Prioritize risks that matter
Not every identified risk should be under your radar, and for that, you must analyze how likely it is to occur and what the potential consequences are. This helps with better prioritization and resource allocation. The best way forward for this exercise is to use a risk matrix, which scores risks based on severity and impact and provides a quick snapshot of what can significantly impact the organization.
Here’s an example of a visual representation of the risk matrix from Sprinto:

Develop a tactical mitigation plan
The next step is to create a mitigation plan to treat immediate, critical risks that can be expensive to remediate later. Start with risk reduction plans, i.e., measures to address risks before they materialize, such as using automated notification tools, arranging employee training, and investing in measures such as encryption, access controls, and firewalls.
Next, have a contingency plan in place for system outages, clinical device failure, and other adverse events. The measures will include backups and redundant systems, reserves of essential supplies, and so on. It is crucial to have clear policies and procedures for each of these measures.
Other things to include in the plan:
- Governance structure: Roles and responsibilities for implementation, monitoring, incident management, etc.
- Performance metrics: Key Performance Indicators and Key Risk Indicators that will be measured and monitored
- Timelines: The expected timeline for control implementation
- Budget allocation: Resource allocation and budgets
Implement risk control measures
Once the plan is finalized and the required budgets are approved, the implementation phase begins. It involves a combination of administrative, physical, and technical risk control measures.
- Administrative measures include policies and procedures such as access control policies, regular internal audits, and staff training.
- Physical measures include restricting access to server rooms or drug facilities.
- Technical measures include installing antivirus software, automated backups, intrusion detection systems, etc.
Arrange for workforce training
It is important to create a culture where employees can proactively identify and report incidents or any risks to patient safety, data, or compliance. This requires frequent training sessions so they understand the plan, their roles, the importance of risk management, and how to respond to risks.
Work on documentation and reporting
Documenting and reporting on risk assessments, mitigation strategies and measures is crucial for compliance purposes and senior management updates. It helps them review the efforts, compare results, and make well-informed decisions for future enhancements.
Monitor and improve
Establish a continuous monitoring mechanism to review the plan’s effectiveness and risk management initiatives. Leverage tools with real-time dashboards to understand the risk posture and analyze metrics. Use data and feedback from stakeholders to iterate the plan as needs evolve.
Check out how Sprinto can help with integrated risk management:
Risk Management in Healthcare Examples
Risk management in healthcare is achieved through developing the right policies and procedures and employing technological solutions to avoid, reduce, or mitigate the risk.
Here are some examples of risk management in healthcare:
| Type of risk | Example | Risk Mitigation |
| Compliance risks | HIPAA violations | Staying updated with healthcare regulationsConducting regular internal audits to ensure adherence |
| Data security risks | Unauthorized access to patient data | Implementing Role-based access controlsConducting access reviews |
| Technological risks | System downtime | Maintaining backup and redundancy systems for IT infrastructure |
| Financial risks | Billing errors | Automating billing processesProviding training for billing and coding |
| Operational risks | Equipment failure | Regular maintenance proceduresPeriodic quality inspections |
| Patient safety risks | Medication errors | Implementing electronic prescribing systems |
| Reputational risks | Publicized data breach | Creating an incident response planEnsuring timely and transparent communication during breaches |
Manage healthcare risks and compliance from one place with Sprinto
While we’ve discussed the importance of managing risks and explored organizational strategies, it’s crucial to recognize that risks don’t exist in silos. They are deeply interconnected—not just with one another but also with key components like governance and compliance. Taking a comprehensive GRC approach broadens your perspective, ensuring well-rounded patient care while maintaining robust defenses and adhering to essential regulations—tools like Sprinto simplify this process, making effective risk management and compliance seamless.
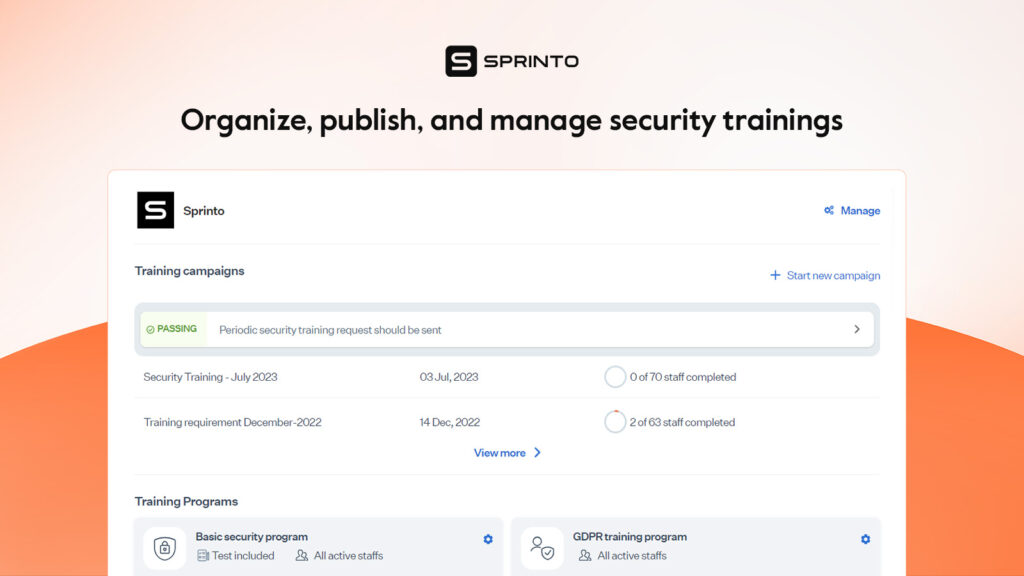
Sprinto is purposely built to help you manage GRC for healthcare and other sectors with minimal lift.
The platform lets you manage roles and responsibilities, organization charts, policies (with in-built templates), reports, reviews, and even change management from one place for solid governance.
As for risk management, Sprinto has:
- A risk library that features most risks faced by cloud-based companies. It also lets you add any custom risks
- Automated risk assessments with risk severity scores, mitigation actions and residual risk analysis.
- You can assign these risks to specific risk owners for role-based remediation
- Detailed risk reports and visual elements make things easier to comprehend and enable the management to make well-informed decisions.
It also provides sweeping coverage across healthcare compliance frameworks like HIPAA, ISO 27001, or SOC2. Built-in training modules, continuous control monitoring, automated evidence collection, and centralized documentation transform months of work into tasks that can be completed in just weeks.
Want to know more about how we can help? Let’s hop on a call to understand each other better.
FAQs
What is the role of a risk manager in healthcare organizations?
Risk managers in healthcare organizations are responsible for conducting risk assessments, developing mitigation strategies, promoting patient care, collaborating for compliance and ensuring ongoing improvements.
How does GRC enhance risk management in healthcare?
GRC in risk management for healthcare helps centralize risk management efforts, integrate risks with compliance, ensure alignment with broader goals through governance, and enhance patient outcomes. It also provides a well-rounded approach to data security and optimizes resource utilization.
Can you guide me on some certifications around risk management in healthcare?
Here are some certifications for risk management in healthcare that you can consider:
- Certified Professional in Healthcare Risk Management (CPHRM) – American Hospital Association
- Certified Risk Management Professional (CRMP) – Risk and Insurance Management Society (RIMS)
- Certified in Healthcare Compliance (CHC) – Health Care Compliance Association (HCCA)
- Certified Healthcare Safety Professional (CHSP) – Board of Certified Hazard Control Management (BCHCM)
What are risk management positions in healthcare?
Risk management positions in healthcare are responsible for identifying, analyzing and mitigating risks related to operations, patient care or compliance. Some key positions include:
- Risk manager: Oversees the implementation of the risk management programs
- Compliance officer: Ensures compliance with healthcare laws
- Patient Safety Manager: Ensures implementation of processes that enhance patient care
- Chief Risk Officer: Oversees the development and implementation of risk management strategies
Payal Wadhwa
Payal is your friendly neighborhood compliance whiz who is also ISC2 certified! She turns perplexing compliance lingo into actionable advice about keeping your digital business safe and savvy. When she isn’t saving virtual worlds, she’s penning down poetic musings or lighting up local open mics. Cyber savvy by day, poet by night!
Related blogs
research & insights curated to help you earn a seat at the table.
















